Medical Reports
Add your latest medical report to keep your health records up to date.Muscular System
Generated: Apr 30, 2025Identification Data and Clinical Context
Service performed:
Musculoskeletal ultrasound – left legOperator:
Dr. Iorgoveanu Stoian Vasilia – Regina Maria, Policlinica The LightHistory:
Pain appeared during recreational jogging (03/30/2025)Examination date:
April 1, 2025, 11:55Method:
High-resolution ultrasound, dynamic and static evaluation
Technical Imaging Details
The examination was performed using the Logiq S7 Expert equipment with 8-12 MHz linear probe, in complementary modes:
- B‑Mode gray‑scale: allows detailed evaluation of anatomical structure and tissue integrity.
- Power Doppler: evaluates blood flow and vascularization to identify areas with hyperperfusion associated with inflammation.
- Elastografie: measures tissue stiffness/elasticity, useful in evaluating muscle injuries.
Imaging Summary

More Details
Your latest check-ins, tests, and updates.| Structure | Appearance on Apr 01, 2025 | Interpretation | Health Status |
|---|---|---|---|
| Myotendinous junction medial gastrocnemius |
Hypoechoic area 1.24 × 0.33 cm Edematous, irregular margins |
Minimal fibrillar tear (grade I) | Acute Lesion |
| Tibio-talar & talo-navicular joints |
No synovitis, no effusion Normal joint space |
Normal appearance, no intra-articular inflammation |
Normal |
| Posterior tibial, peroneal, toe flexor, Achilles tendons |
No tenosynovitis Normal echogenicity, preserved thickness |
Intact tendons, no signs of inflammation |
Normal |
| Ligaments (deltoid, lateral, Spring) |
Intact, normal fibrillar architecture No hypoechoic areas |
Intact ligamentous structures | Normal |
Lesion Classification Details
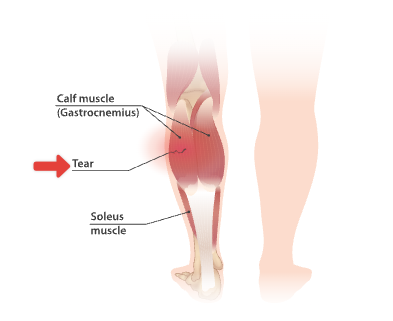
Read LessClassification of muscle tears:
Grade I
present in patient
< 5% of muscle fibers torn, muscle architecture generally preserved, no visible defect
Grade II
5-50% of muscle fibers affected, visible defect, but with partial maintenance of continuity
Grade III
> 50% of fibers affected, complete fascicle rupture, evident muscle retraction
Ultrasound criteria for grade I lesions:
- Focal hypoechoic area with dimensions under 2 cm
- Preserved perilesional muscular fibrillar architecture
- Absence of collected hematoma
- Minimal or absent Doppler hypervascularization
Coding and Diagnostic Codes
primary code:
- ICD-10 T09.08 - Other superficial injury of trunk, level unspecified
secondary codes:
- ICD-10 S96.1 - Injury of muscle and tendon of other muscles at ankle and foot level
- RMIS 37.2.14 - Minimal gastrocnemius lesion
Important Note
Although the lesion is minor (grade I), neglecting adequate treatment or prematurely resuming intense physical activity increases the risk of transformation into a chronic lesion or worsening to grade II. Strict adherence to recovery recommendations is essential.
Clinical Significance
Grade I
Grade I fibrillar tears (< 5% fibers torn) of the medial gastrocnemius frequently occur due to excessive strain during sports activities or sudden dorsiflexion movements.
The size of ~1.2 cm suggests a very small lesion with good healing potential.
Recovery Period
2-6 Weeks
Depending on symptom control and rehabilitation compliancePrognosis
Excellent
Risk of complications < 10%, chances of complete healing > 95%Predictable evolution based on medical literature:
Pain Reduction
75% in 10-14 days
Edema Reduction
90% in 14-21 days
Muscle strength recovery
90-100% in 4-6 weeks
Estimated Evolution
-
Apr 1, 2025 USG diagnosis and PEACE protocol initiation.
Day 0
Present- Protection - reducing painful movements
- Elevation - positioning the limb to reduce edema
- Avoid anti-inflammatories (NSAIDs) - may interfere with the initial healing phase
- Compression - elastic bandage to limit edema
- Education - informing the patient about pathology and evolution
-
Apr 7-10, 2025 Clinical check-up, indicative ultrasound: confirmation ↓edema, initiation of light LOVE exercises
Week 1
- Load - isometric exercises without pain
- Optimism - positive approach to recovery
- Vascularization - stimulating local blood flow
- Exercise - specific rehabilitation protocol
-
Apr 15-28, 2025 Functional re-evaluation; increased eccentric loading, possible light jogging
Week 3-4
- Assessment of muscle strength and elasticity
- Functional testing (unipodal, light jumps)
- Initiation of low-intensity plyometric exercises
- Light jogging over short distances (500-1000m)
-
May 6-12, 2025 Final ultrasound; reintegration into sport/full effort if integrity is demonstrated
Week 6
- Final imaging assessment
- Complete functional testing
- Resumption of full sports activities if parameters are normal
- Prevention plan to avoid recurrences
Favorable Factors
The following factors predict a favorable evolution in your case:
- Protection - reducing painful movements
- Elevation - positioning the limb to reduce edema
- Avoid anti-inflammatories (NSAIDs) - may interfere with the initial healing phase
- Compression - elastic bandage to limit edema
- Education - informing the patient about pathology and evolution
Immediate Recommendations
Protocol PEACE & LOVE based on the latest recommendations (Br J Sports Med. 2024)- Protection - Limit movements that cause pain in the first 72h
- Elevation - Keep the limb elevated to reduce swelling
- Avoid anti-inflammatories - NSAIDs can slow down natural healing
- Compression - Use an elastic bandage to control swelling
- Education - Understand the natural healing mechanisms and evolution
- Load - Gradual introduction of active exercises without pain
- Optimism - A positive attitude stimulates healing processes and adherence
- Vascularisation - Aerobic activities stimulate healing
- Exercise - Recovery of function through specific guided exercises

Recommended Medication
Read LessMedication
Related on the patient’s condition| MEDICATION | DOSAGE | INDICATIONS | OBSERVATIONS |
|---|---|---|---|
| Paracetamol | 500mg, 1-2 tablets every 6 hours | Mild-moderate pain | Preferred analgesic in the initial phase |
| Diclofenac gel 1% | Local application 2-3 times/day | Localized pain | Only after 72h from trauma |
| Diosmin/Hesperidin | 1000mg/day, 7-10 days | Post-traumatic edema | Optional, anti-edema adjuvant |
Important Note
Oral NSAIDs (Ibuprofen, Naproxen, etc.) are not recommended in the first 72h, as they can interfere with natural tissue healing processes.
Physiotherapy Protocol
Read Less-
Day 1-5
Phase I
- Relative rest avoiding painful movements
- Short cryotherapy (<10 min/session, 2-3 sessions/day)
- Submaximal isometric contractions at 0° knee flexion
- Painless active ankle mobilization
-
Day 6-14
Phase II
- Light isotonic exercises in supine position
- Gentle static passive stretching (<30 sec, 3 repetitions)
- Proprioceptive exercises in non-weight bearing
- TENS electrostimulation for pain control (optional)
-
Week 2-4
Phase III
- Eccentric exercises with progressive resistance
- Closed kinetic chain exercises
- Dynamic stretching and neuromuscular facilitation
- Initiation of light functional activities
-
Week 4-6
Phase IV
- Progressive plyometric exercises
- Sport-specific functional training
- Recurrence prevention protocol
- Full reintegration into previous activities
Image Monitoring
Read Less
Recommended imaging evaluation schedule:
Intermediate control ultrasound
Day 10-14- Assessment of edema reduction
- Verification of absence of complications
- Adjustment of the therapeutic plan according to evolution
Final ultrasound
Week 5-6- Confirmation of complete healing
- Assessment of scar tissue quality
- Decision to resume full activity
Technical recommendations:
Use of the same device, probe, and examiner for optimal comparability; standardized positioning; evaluation in static and dynamic conditions.
Pharmacies Near You
Here is the list of all pharmacies near you
Farmacia Dr. Max
Calea București 104, 620m Non-StopFarmacia Regina Maria
Strada Aurel Vlaicu 62-64, 780m Open 08:00 - 20:00Farmacia Catena
Strada Otopeni 22, 350m Open 08:00 - 22:00Complementary Natural Treatments
Recommended imaging evaluation schedule:
Role of Natural Therapies
Natural therapies can be used as an adjunct to conventional medical treatment, but do not replace it. Recent studies indicate the potential of some natural remedies in reducing inflammation and improving tissue healing processes.
Always consult your doctor before starting any natural therapy to avoid unwanted interactions.
Moderate evidence level
Phytotherapy
Arnica montana
Topical applications (cream/gel/diluted tincture) 2-3 times/day to reduce local edema and inflammation. Avoid application on broken skin.Boswellia serrata
Standardized extract (300-400mg 3 times/day) for natural anti-inflammatory properties. Effect observable after 7-10 days of administration.Curcumina
Extract from turmeric - 500mg 2 times/day, with high bioavailability formulation, to reduce inflammation and oxidative stress.
Moderate evidence level
Acupuncture
Traditional Chinese acupuncture can accelerate recovery by:- Stimulating local blood flow
- Reducing pain by stimulating endorphin release
- Modulating the inflammatory response
Recommendation
Recommendation: 1-2 sessions/week in the subacute phase (after the first 72h), with an accredited therapist. Main points used: GB-34, SP-6, ST-36, LV-3, plus local points depending on individual assessment.
Moderate evidence level
Essential Oils
Recommended blend for topical applications (diluted in carrier oil 3-5%):- Lavender oil - anti-inflammatory and analgesic properties
- Rosemary oil - stimulates local circulation
- Peppermint oil - cooling and analgesic effect
Recommendation
Apply by gentle massage around the affected area (not directly on the lesion) 1-2 times/day. Always test on a small patch of skin before use to check for adverse reactions.
Moderate evidence level
Natural Supplements
Hydrolyzed collagen
10-15g/day to support connective tissue regeneration. Studies show increased efficacy when associated with vitamin C.Bromelain
500-1000mg/day between meals, for anti-inflammatory properties and improved edema absorption. Contraindicated in case of pineapple allergies.Antioxidant complex
Vitamin C (500-1000mg/day), Vitamin E (200-400 IU/day) and Zinc (15-30mg/day) to reduce oxidative stress and stimulate healing processes.Medication and Relaxation Techniques
Read Less
Relaxation techniques that can accelerate the healing process by reducing stress and optimizing the immune response:
Studies show that stress reduction techniques can significantly improve recovery speed after musculoskeletal injuries by modulating the inflammatory response and optimizing metabolic processes.
- Diaphragmatic breathing - 5-10 minutes, 2-3 times/day
- Body scan meditation (Body Scan) - 15-20 minutes daily
- Guided imagery for healing - 10 minutes before bedtime
Traditional Chinese Medicine
Read Less
From the perspective of traditional Chinese medicine, muscle injuries involve stagnation of Qi and blood (Yu Xue) in the affected meridians.
Recommended traditional formulas:
- Yunnan Baiyao - classic formula for trauma, promotes blood circulation and reduces edema
- Die Da Wan - for relieving pain and inflammation associated with traumatic injuries
- Jin Gu Die Shang Wan - for repairing tendons and ligaments
Important Note
Use these remedies only under the supervision of a qualified practitioner of traditional Chinese medicine, as dosage and indications may vary depending on individual energy diagnosis.
Ayurvedic Therapies
Read Less
According to Ayurveda, muscle injuries involve an imbalance of Vata and Pitta doshas. Ayurvedic remedies focus on restoring this balance:
Recommended traditional formulas:
- Ashwagandha (Withania somnifera) - 300-500mg 2 times/day for anti-inflammatory and adaptogenic effects
- Boswellia - 300-400mg 3 times/day for inflammation reduction
- Sesame oil - for local massage (Abhyanga), having Vata-calming properties
- Kati Basti - local application of warm medicated oil
- Pinda Sweda - warm boluses with medicinal herbs for inflammation reduction
Important Precautions
When using complementary natural therapies, consider the following:
- Inform your attending physician about all natural remedies used
- Check for potential interactions with prescribed medications
- Stop administration at the first signs of adverse reactions
- Choose standardized products from trusted manufacturers
- Do not discontinue conventional medical treatment in exclusive favor of natural therapies
Nutritional Recommendations
Optimal nutrition can accelerate tissue healing processes. Recommendations:- Quality proteins (1.5-2g/kg/day) - essential for tissue regeneration
- Anti-inflammatory foods - fatty fish, nuts, seeds, olive oil, berries
- Foods rich in Vitamin C - citrus fruits, bell peppers, kiwi, broccoli (support for collagen synthesis)
- Foods rich in Zinc - pumpkin seeds, lean meat, seafood (accelerates healing)
- Adequate hydration (2-3L/day) - optimizes circulation and cellular metabolism
- Limit alcohol and sugar - can delay healing processes and increase inflammation
Advanced Investigations and Procedures (optional)
For persistent lesions > 6 weeks or high-performance athletes, advanced therapeutic options based on the latest discoveries in sports medicine are available:US‑MRI fusion tracking
State-of-the-art technology for quantifying muscle scarring and guiding return to sport. Recent studies (ECR 2024)2 demonstrate superior accuracy in assessing repair tissue quality and re-rupture risk.PRP Infiltration
Ultrasound-guided injection with platelet-rich plasma (2–4 ml, 1 session). 2024 Meta-analysis: moderate evidence for reducing recovery time by approximately 30% in active athletes.Implantable wireless EMG electrodes
Research technology for personalized biofeedback in rehabilitation. Provides real-time data on muscle activation and allows precise adjustment of the recovery program. Available in clinical trials at university centers.
Important
The advanced procedures mentioned are not necessary in your case, given the minimal grade lesion and expected favorable evolution. They are presented for complete information and could be considered only in case of unfavorable evolution or for high-performance athletes needing accelerated recovery.
Follow-up and Progression Plan
Protocol PEACE & LOVE based on the latest recommendations (Br J Sports Med. 2024)-
April 10, 2025 Clinical evaluation by sports physician/orthopedist to check progress and adjust treatment.
Clinical Check-up
Dr. Popescu MihaiApril 10, 2025, 2:30 PMPoliclinica Regina Maria021.xxx.xxxx -
April 15, 2025 Assessment session and initiation of the specialized recovery protocol.
Physiotherapy Assessment
Dr. Popescu MihaiApril 10, 2025, 2:30 PMPoliclinica Regina Maria021.xxx.xxxx -
April 22, 2025 Imaging assessment to monitor lesion evolution and adjust the therapeutic plan.
Control Ultrasound
Dr. Popescu MihaiApril 10, 2025, 2:30 PMPoliclinica Regina Maria021.xxx.xxxx -
May 13, 2025 Complete assessment (clinical and imaging) for the decision to reintegrate into activities and sports.
Final Assessment
- Clinical assessment + ultrasound
- Functional testing (LEFS)
- Prevention plan to avoid recurrences
LEFS Functional Scale
At each visit, the Lower Extremity Functional Scale (LEFS) will be completed - a validated 20-question questionnaire for objective assessment of functional progress. The maximum score is 80 points.
- Initial: 45-50 points
- After 2 weeks: 60-65 points
- After 4 weeks: 70-75 points
- At 6 weeks: >75 points (complete recovery)
Indications for Further Investigations
A 3T MRI (high-resolution magnetic resonance imaging) will be performed if:
- Pain or functional deficit persists after 6 weeks
- Clinical or imaging deterioration occurs during the recovery period
- There is suspicion of initially undetected associated lesions
Detailed Recovery Plan
Recommended imaging evaluation schedule:Temporarily Restricted Activities
The following activities should be avoided in the first 2 weeks:- Running, jumping, impact activities
- Intense or forced stretching of the gastrocnemius group
- Exercises with high eccentric loading (repetitive stair descent)
- Sports activities involving sudden changes of direction
Immediately Permitted Activities
The following activities are safe and beneficial from the first week:- Normal walking within comfort limits (without limping)
- Swimming or hydrotherapy (without strong leg push)
- Stationary cycling with minimal resistance
- Exercises for the upper body and unaffected limbs
Recommended Functional Progression:
Check the progression according to phases| PHASE | TIMING | objectives | permitted activities |
|---|---|---|---|
| Phase I | Days 1-7 | Limiting inflammation Protecting the affected area |
Normal walking Isometric exercises Cryotherapy |
| Phase II | Week 1-2 | Restoring mobility Initiating gradual loading |
Light isotonic exercises Gentle passive stretching Stationary cycling |
| Phase III | Week 2-4 | Increasing strength Functional training |
Eccentric exercises Balance training Light jogging on flat surfaces |
| Phase IV | Week 4-6 | Preventing recurrences Full reintegration |
Plyometric exercises Sport-specific training Full physical activity |
Recommended exercises initial phase
Read LessIsometric gastrocnemius contractions:
- In a sitting position, with the knee at 90°
- Press the foot down without moving the ankle
- Hold the contraction for 5-10 seconds
- Repeat 10-15 times, 3 times/day
Active ankle mobilizations:
- Dorsal and plantar flexion within painless limits
- Circular ankle movements
- 20 repetitions, 3-4 times/day
Isometric contraction in standing:
- Standing, with support on both feet
- Gently press the affected foot into the floor
- 5-10 seconds contraction, 10-15 repetitions
Important
All exercises must be performed without pain. Stop immediately if pain occurs.
Progression Criteria
Progress to the next recovery phase only when all criteria are met:
- Absence of pain in current activities
- Minimal or absent edema
- Normal gait, without limping/li>
- Achievement of specific objectives of the current phase
- Clinical or imaging confirmation of favorable evolution
Patient Goals
This section reflects your personal recovery goals and preferences as discussed with the medical team. The treatment plan will be adapted to support achieving these targets safely and effectively.Your Recovery Goals
-
Next 2-4 weeks
Short-Term Goals
- Complete pain reduction during normal walking and light daily activities.
- Walking without a limp for distances up to 1 km.
- Ability to ascend and descend stairs alternating legs, without pain.
- Initiation of light treadmill jogging (5-10 minutes) by the end of the period. (Discussed on 03/30/2025)
-
Next 4-8 weeks
Long-Term Goals
- Return to regular recreational running (3-5 km, 2-3 times/week) without pain or discomfort. (Discussed on 03/30/2025)
- Participation in medium-difficulty mountain hikes.
- Full regain of strength and flexibility in the left leg, comparable to the right.
Your Treatment Preferences
Based on previous discussions, the following preferences were noted:- Preference for an active recovery program with direct involvement in exercises.
- Openness to using complementary therapies (e.g., acupuncture, phytotherapy) as an adjunct, if considered safe and beneficial.
- Desire to minimize the use of oral anti-inflammatory drugs, preferring local or alternative approaches for pain management.
- Importance of receiving detailed information and continuous education throughout the recovery process.
Update
These goals and preferences will be periodically re-evaluated and adjusted based on recovery progress and any new medical information.
Patient Education
Learn more about your health, treatments, and how to stay well.What is a fibrillar tear?
Read Less- Localized pain, intensified by muscle contraction
- Local edema (swelling) due to inflammation
- Tenderness to palpation at a specific point
- Possible discreet hematoma (only in some cases)
How does a fibrillar tear heal?
Read LessInflammatory phase (Days 0-5):
- Dilated blood vessels allow access for inflammatory cells
- Macrophages "clean" the area of damaged fibers
- This phase is essential and should not be completely suppressed
Proliferative phase (Days 5-14)
- Formation of new capillaries in the affected area
- Migration of satellite cells for fiber regeneration
- Collagen deposition for structural support
Remodeling phase (Day 14 - Week 8)
- Reorganization of collagen fibers along the lines of force
- Maturation of scar tissue
- Progressive restoration of biomechanical properties
Why is rehabilitation important?
Read Less- Optimizing healing quality - New muscle fibers and scar tissue organize according to applied forces
- Preventing atrophy - Unused muscles can lose up to 3% of their mass per day of immobilization
- Restoring flexibility - Scar tissue tends to be less elastic than normal muscle tissue
- Preventing recurrences - Recurrence rate can reach 30% without adequate rehabilitation
- Relearning motor patterns - Neuromuscular reprogramming for efficient and safe movements
When to return urgently?
Read Less- Sudden severe pain - May indicate tear extension
- Progressive edema - Swelling that worsens instead of improving
- Increased local temperature, intense redness - Possible sign of infection or complication
- Inability to bear weight on the limb - Suggests worsening of the lesion
- Changes in color or sensation in the foot - May indicate vascular or neurological problems
How to prevent recurrences?
Read Less- Adequate warm-up - Minimum 10-15 minutes before intense physical activity
- Regular stretching program - Optimal flexibility reduces the risk of injuries
- Gradual increase in intensity - Avoid sudden increases in intensity or volume (10% rule)
- Muscle strengthening - Specific strength exercises for the entire kinetic chain
- Hydration and nutrition - Essential for optimal muscle function
- Rest and recovery - Respect recovery periods between intense sessions
- Adequate equipment - Footwear appropriate for the sport and your anatomy
Frequently Asked Questions
Find quick answers to common questions.Question:
Can I use ice or heat for my injury?Answer:
Ice can be applied in the first 24-72 hours for short periods (<10 minutes) to reduce pain. After the acute phase, moderate heat can stimulate circulation and healing. Avoid both temperature extremes and do not apply directly to the skin.Question:
Can massaging the area help with recovery?Answer:
Direct massage on the injured area should be avoided in the first 7-10 days. After this period, gentle massage performed by a specialist can help reduce muscle tension and stimulate circulation.Question:
Is surgery needed for this type of lesion?Answer:
No, grade I fibrillar tears do not require surgical intervention. Conservative (non-surgical) treatment has excellent results, with complete recovery in most cases.Question:
When can I return to sports/running?Answer:
Return to sports should be gradual and guided by the absence of pain. For light jogging, usually in weeks 3-4, and for full sports in weeks 5-6, after the final assessment.Useful Tips
Find quick answers to common questions.- Maintain adequate general physical activity even during the recovery period - avoid complete sedentary behavior
- Hydrate properly - dehydration increases the risk of muscle injuries
- Ensure an adequate protein intake (1.2-1.6g/kg/day) to support tissue recovery
- Keep a journal of symptom evolution and functionality to monitor progress
- Do not compare your recovery with others - the healing process varies individually
Bibliography and References
- Dubois B, Esculier JF. A stronger evidence base is needed for therapy in soft tissue injuries. Br J Sports Med. 2024;58(3):136-144.
- European Society of Radiology. US‑MRI fusion exploration allows assessment of injury healing – EPOS C‑24079, ECR 2024. European Congress of Radiology, Vienna, 2024.
- American Institute of Ultrasound in Medicine. AIUM Practice Parameter for the Performance of a Musculoskeletal Ultrasound Examination. 2024 update. J Ultrasound Med. 2024;43(2):301-328.
- Thompson N, Schache A, Comfort P, et al. Dynamic tissue healing: New paradigms in soft tissue rehabilitation. Physical Therapy in Sport. 2024;59:102-114.
- Medscape. New guidance clarifies use of musculoskeletal ultrasound 2024. Medscape Medical News, February 15, 2024.
- International Consensus Group on Muscle Injuries. Consensus statement on muscle injuries: improving diagnosis, healing assessment, and return to sport decision. Sports Med. 2023;53(10):1689-1704.
Additional Resources
Educational materials and additional information available online:
- Exercise guide for gastrocnemius injury recovery (Romanian Society of Sports Medicine)
- Muscle injury prevention program for amateur athletes
- "RehApp" mobile application for monitoring and guiding muscle recovery
Risk Factors
Understanding the factors contributing to muscle injuries is crucial for their prevention. These can be divided into intrinsic (individual-related) and extrinsic (environment and activity-related) factors.Intrinsic Risk Factors
Read Less- Age: Muscle elasticity decreases with age. The patient (48 years) falls into a category with slightly increased risk.
- Previous injuries: A previous injury increases the risk of a new one. (Unknown in this case, to be assessed)
- Reduced flexibility: Stiff muscles are more prone to tears. (To be specifically assessed for the gastro-soleus group)
- Muscle imbalances: Strength differences between muscle groups (e.g., quadriceps vs. hamstrings, or between limbs).
- Inadequate muscle strength: Especially eccentric strength of the calf muscles.
- Poor biomechanics: E.g., excessive pronation, inefficient running pattern. (Requires podometric and running technique assessment)
Extrinsic Risk Factors
Read Less- Training errors: Sudden increases in jogging intensity, duration, or frequency. (Relevant in the patient's case)
- Insufficient warm-up: Inadequate muscle preparation for effort.
- Fatigue: Fatigued muscles absorb less shock and are more vulnerable.
- Improper equipment: Worn-out running shoes or unsuitable for pronation type.
- Training surface: Running predominantly on hard surfaces (asphalt) can increase impact.
- Environmental conditions: Running in cold weather without adequate warm-up.
General Prevention Strategies for Calf Injuries
- Dynamic Warm-up: Include calf-specific exercises (e.g., toe walks, heel walks, light jumps).
- Progressive Strengthening: Regular exercises for gastrocnemius and soleus muscles (e.g., calf raises with straight and bent knee, with and without weights).
- Eccentric Training: Crucial for stretch resistance (e.g., slow heel drops off a step).
- Regular Stretching: Maintaining calf and Achilles tendon flexibility. Both static and dynamic stretching.
- Gradual Training Progression: Adherence to the 10% rule (do not increase volume/intensity by more than 10% per week).
- Appropriate Footwear Choice: Replace running shoes every 500-800 km and choose models appropriate for foot biomechanics.
- Varying Running Surfaces: Alternate running on asphalt with softer surfaces (dirt, grass, track).
- Rest and Recovery: Include active or complete rest days in the training program.
Helpful Tip
Implementing these strategies can significantly reduce the risk of calf muscle injuries and improve long-term athletic performance.
Genetic Data and Relevant Biomarkers
Understanding an individual's genetic profile and monitoring specific biomarkers can provide valuable insights into injury predisposition, training response, and the recovery process. This section presents hypothetical data and reference values. Genetic information is complex and its interpretation requires specialized consultation. Biomarkers must be correlated with the clinical context.Genetic Markers Associated with Musculoskeletal Health (Hypothetical Examples)
Read LessGene and Implications
Check out the general recommendation depending on the gene| GENE (SNP) | patient genotype | potential implication | General Recommendation |
|---|---|---|---|
|
COL1A1
(rs1800012)
|
G/T | Slightly increased risk for connective tissue injuries. | Emphasis on warm-up, stretching, collagen/vit. C intake. |
|
COL5A1
(rs12722)
|
C/C (normal) |
Normal profile for type V collagen integrity. | Maintain active lifestyle. |
|
ACTN3
(rs1815739)
|
R/X |
Mixed profile for performance (power/endurance). Moderate risk of muscle injury with explosive effort. |
Balanced training, caution with strength exercise progression. |
|
IL-6
(rs1800795)
|
G/G (normal) |
Normal inflammatory response. | Standard post-exercise inflammation monitoring. |
Relevant Blood Biomarkers | Lab Tests
Blood Biomarkers
Check out the general recommendation depending on the gene
Values until
04/02/2025
| BIOMARKER | patient VALUE | Reference Range | Unit | Interpretation |
|---|---|---|---|---|
|
C-Reactive Protein (CRP)
|
6.5 | < 5.0 | mg/L | Slightly elevated (inflammation) |
|
Creatine Kinase (CK)
|
450 | 30 - 200 | U/L | Elevated (muscle damage) |
|
Vitamin D (25-OH)
|
35 | 30 - 100 | ng/mL | Optimal level |
|
Ferritin
|
120 | 30 - 400 | ng/mL | Normal iron stores |
|
Lactate Dehydrogenase (LDH)
|
250 | 135 - 225 | U/L | Slightly elevated (possible exertion) |
Lifestyle and Ergonomic Considerations
Adapting daily activities, the work environment, and sleep habits can significantly facilitate recovery, prevent overuse of the injured area, and contribute to overall well-being.Adapting Daily Activities
Read Less- Stair climbing: In the initial phase (first 1-2 weeks), lead with the healthy leg when going up and with the affected leg when going down ("good leg to heaven, bad leg to hell"). Use the handrail. Limit frequency if pain occurs.
- Prolonged standing: Alternate weight-bearing, perform light ankle movements (flexion/extension) every 20-30 minutes. Consider using an anti-fatigue mat.
- Driving: Ensure you can operate pedals painlessly and with full control, especially the accelerator/brake for the left foot (if applicable for manual transmission or adapted controls). Adjust seat position to minimize calf strain.
- Footwear choice: Wear comfortable shoes with good arch support and adequate cushioning. A slightly elevated heel (1-2 cm) may initially reduce strain on the gastrocnemius. Avoid high heels or completely flat shoes without support long-term.
- Household chores: Avoid activities involving standing on tiptoes or excessive calf stretching (e.g., reaching for high shelves). Ask for help if needed.
Workplace Ergonomics
Read LessFor office work (predominantly seated):
- Adjust chair height so thighs are parallel to the floor and feet are fully supported.
- Use a footrest if feet do not comfortably reach the floor, to keep knees at approximately a 90° angle.
- Take short breaks (1-2 minutes) every 30-60 minutes to stand up, walk a bit, and perform light calf stretches.
- Consider using an adjustable-height desk (standing desk) to alternate between sitting and standing periods.
For work involving prolonged standing or physical exertion:
- Wear appropriate protective footwear with good cushioning and support.
- Use anti-fatigue mats if standing for long periods on hard surfaces.
- Use correct techniques for lifting and carrying weights (bend knees, keep back straight).
- Avoid sudden, twisting, or repetitive movements that strain the calves.
Importance of Sleep for Recovery
Quality sleep is essential for tissue repair processes and inflammation modulation. Growth hormone, crucial for healing, is predominantly released during deep sleep. Insufficient or poor-quality sleep can delay recovery.Tips for restful sleep:
- Maintain a regular sleep schedule (go to bed and wake up at the same times, even on weekends).
- Create an optimal sleep environment: dark, quiet, comfortable temperature (ideally 18-20°C / 64-68°F).
- Avoid caffeine and alcohol at least 4-6 hours before bedtime.
- Limit screen exposure (phone, tablet, TV) 1-2 hours before sleep.
- Adopt a relaxing bedtime routine (e.g., reading, warm bath, light meditation).
Emotional Support and Coping Strategies
Emotional well-being is an important predictor of successful physical recovery. A proactive approach to mental health can accelerate healing and improve quality of life throughout this process.- Acknowledge emotions: Allow yourself to feel and process these emotions without self-judgment.
- Education and understanding (self-efficacy): Detailed knowledge of the injury, healing process, and recovery plan increases a sense of control and reduces anxiety.
- Setting realistic and flexible goals: Break down recovery into small, achievable steps (SMART goals). Be prepared to adjust goals if necessary.
- Maintaining a positive outlook (Optimism): Focus on the progress made, however small, not on temporary limitations. Visualize successful recovery.
- Stress management techniques: Incorporate relaxation techniques, mindfulness, meditation, or deep breathing into your daily routine.
- Activating social support network: Communicate openly with family, friends, teammates, or other athletes who have had similar experiences.
- Maintaining engagement in activities (adapted): Find ways to stay involved in hobbies, work, or social life, even if it requires adaptations
- Seeking professional support: If emotional difficulties persist or become overwhelming, do not hesitate to consult a sports psychologist, therapist, or counselor.
Cost Estimates
This section provides indicative information regarding estimated costs for certain investigations and procedures, as well as relevant reimbursement codes. These are general estimates and may vary.Estimated Costs for Recommended Services
Check out the estimated costs.| SERVICE/PROCEDURE | ESTIMATED COST | NOTE |
|---|---|---|
| Initial Musculoskeletal Ultrasound | 300 - 500 RON | Performed on 04/01/2025 |
| Consultation Specialist Orthopedics/Sports Medicine | 250 - 450 RON / consultation | Initial and final check-up recommended |
| Physiotherapy/Kinesiotherapy Session | 150 - 250 RON / session | Estimated 8-12 sessions over 4-6 weeks |
| Follow-up Musculoskeletal Ultrasound | 250 - 400 RON / session | 1-2 follow-ups recommended |
| PRP Infiltration (optional, if applicable) | 800 - 1.500 RON / procedure | Discussed as advanced option |
| Blood tests (CRP, CK, etc.) | 100 - 300 RON / set | Depending on requested panel |
Important Note
The costs presented are estimates and may differ based on location, case complexity, healthcare provider, and your specific insurance policy coverage. For exact information, please contact the healthcare provider and your insurance company directly.
Insurance and Reimbursement Information
Medical cost coverage depends on your insurance policy type (public - CAS, or private) and its specific conditions.Recommended steps:
- Check policy coverage: Contact your insurer to understand which services are covered and the settlement/reimbursement procedure.
- Pre-authorization: Some procedures may require pre-authorization from the insurer.
- Partner network: Check if the healthcare provider (clinic, doctor) is in your insurer's preferred network to benefit from preferential rates or direct billing.
Diagnostic and Procedure Codes (Relevant):
- ICD-10 (Diagnosis): See "Diagnosis" section for specific codes (e.g., S96.1).
- CPT (Procedures - USA, indicative example) / Local Codes:
- Musculoskeletal ultrasound: e.g., CPT 76881 (complete), 76882 (limited). Local codes may vary.
- Physiotherapy: e.g., CPT 97110 (therapeutic exercises), 97112 (neuromuscular reeducation). Local codes may vary.
Long-Term Management
Congratulations on completing the acute recovery phase! To maintain the benefits achieved, prevent recurrences, and ensure optimal long-term musculoskeletal health, it is important to adopt and maintain certain healthy strategies and habits.Key Strategies for Maintaining Muscle Health
- Continuation of an adapted exercise program: Regularly include strength (especially eccentric for calves), flexibility, balance, and proprioception exercises. Discuss a maintenance plan with your physiotherapist.
- Self-monitoring and listening to your body: Pay attention to early signs of overuse, discomfort, or pain. Do not ignore these signals; reduce intensity or take a break.
- Smart adaptation of workouts: Gradually modify the intensity, duration, and frequency of activities. Avoid sudden returns to maximum effort levels after periods of inactivity.
- Body weight management: Maintaining a healthy weight reduces stress on joints and muscles.
- Continued nutrition and hydration: A balanced diet rich in protein, vitamins, and minerals supports muscle health. Ensure adequate hydration, especially on days with physical activity.
Periodic Medical Check-ups and When to Seek Help
Routine check-ups:
- An annual check-up with your family doctor or sports physician is recommended for a general health assessment and to discuss any musculoskeletal concerns.
- If you practice sports regularly, a periodic functional assessment by a physiotherapist can help identify imbalances or weaknesses early on.
Seek medical consultation if:
- Pain reappears in the previously injured area, persisting for more than a few days or worsening.
- You notice a new injury or significant discomfort elsewhere in your body.
- You feel persistent weakness, instability, or a functional limitation affecting your daily or sports activities.
- You want to start a new intense physical activity or significantly change your training program and need advice on how to do so safely.
 Regina Maria
Regina Maria
 MedLife
MedLife
 Sanador
Sanador